Systematic review on the technology’s role in supporting lung cancer patients in the treatment journey
The reviewed articles demonstrated high methodological quality (A and B score), primarily using appropriate qualitative approaches and adequate data collection methods. Thus, all studies were included. While all randomized controlled studies showed no selection bias and comparable groups, one faced attrition bias11, and the blinding of assessors was not reported, raising detection bias concerns11. Most non-randomized studies had representative samples, but only a few adequately addressed confounders12,13. Mixed-method studies provided solid rationale and integration of methods, but only one study adequately addressed divergences in results. The entire appraisal results are shown in Supplementary Table 1.
Data extraction and study characteristics
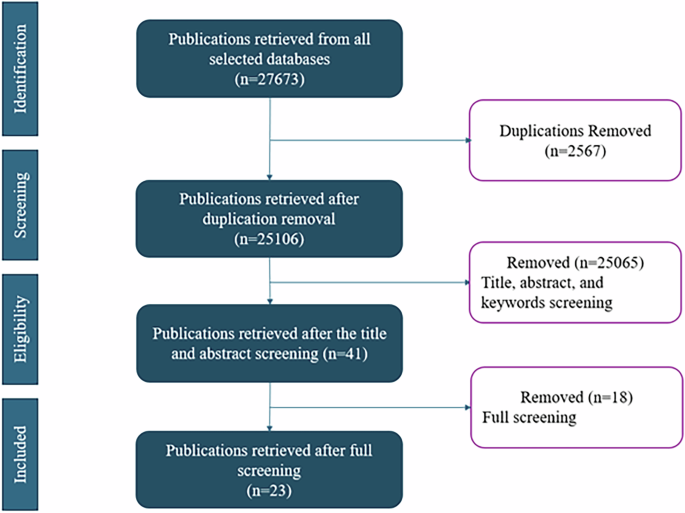
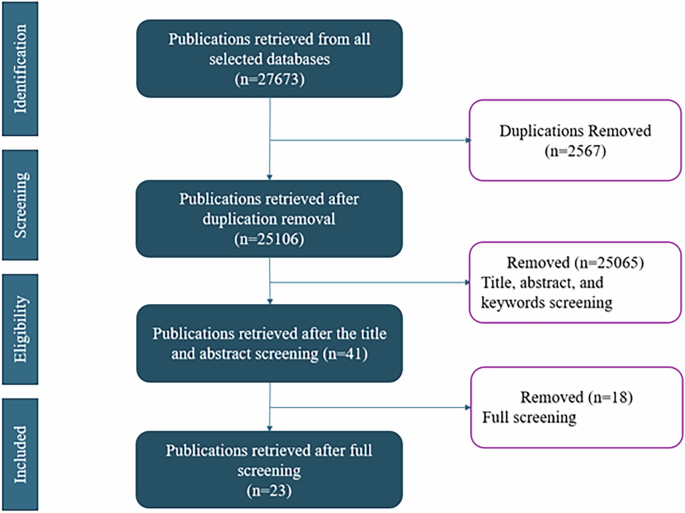
A total of 27673 articles were retrieved from the databases. We included 5345 articles for the title review after removing 2567 duplicates and 209 reviews and meta-analysis. We screened the title and abstract of the studies and found 41 eligible articles. Eventually, we found 23 eligible articles through a full review, as shown in Fig. 1. Figure 2 indicates the yearly distribution of the included studies. Studies included were published between 2007 and 2024, with two studies published before 2010 14,15, 10 published between 2010 and 201912,13,16,17,18,19,20,21,22,23, and 11 published between 2020 and 202411,24,25,26,27,28,29,30,31,32,33. All findings are summarized in Table 1 and Supplementary Table 2.
Summary of the PRISM flow with statistics on the articles included and excluded at each level of the filtering.
Yearly comparison of the articles publication to help track the temporal trends of the studies about technology supporting treatment among lung cancer patients.
Figure 3 maps out the geographic distribution of the countries where the studies were conducted. Eleven studies were conducted in Europe13,16,17,18,19,20,25,27,28,31,32, including four studies in France18,19,25,28, and three studies in the Netherlands16,17,20. Nine studies were conducted in North America, all in the United States11,14,15,21,24,26,29,30,33. Three studies were conducted in Asia12,22,23.

Geographical comparison of the articles publication to help track the locations of the studies about technology supporting treatment among lung cancer patients.
The studies used different technologies, including telehealth (n = 9)11,13,15,18,24,26,28,29,33, online portals (n = 8)12,16,17,20,27, mobile applications or mHealth (n = 8)18,19,21,23,30,31,32, electronic assessment tools (n = 3)13,22,25, and virtual reality (n = 1)14.
Twenty-three interventions were delivered by healthcare providers (HCPs): five studies utilized a multidisciplinary team involving various providers, such as oncologists, physiologists, and nurses16,24,25,27,33, five studies involved nurses13,14,15,21,22,30, six studies involved physicians11,17,18,19,23,26, two studies involved physical therapists24,28, one study involved emergency department HCPs12, and one study resorted to specialized trainers to deliver the intervention sessions29. Primarily, the interventions were delivered in home settings (n = 20)11,12,13,15,16,17,18,19,20,21,23,24,26,27,28,29,30,31,32,33, clinic settings (n = 2)14,22, and in both settings (n = 1)25, with a reported duration ranging from one single session12,19 to up to 30 months25. The median duration of the 25 interventions with a specified delivery length was three months. Seven of the included studies were guided by theoretical frameworks. The theories used were social cognitive theory29, user-centered design principles16, value-based healthcare principles27, chronic care self-management model24, and Lazarus and Folkman’s stress and coping model14.
Study Populations and Treatment Challenges
The study included cancer patients at different stages of the diagnosis. Eight studies included patients with both local and metastatic cancer15,17,18,19,20,21,23,25,26,27,29, eight studies had only patients with advanced-stage or metastatic cancer11,28,30,31,32, one study included only patients with stage I cancer16, and eight studies did not specify the stage of cancer of the study population12,13,14,22,24,33. These patients were undergoing a variety of treatment regimens: 15 included patients undergoing chemotherapy11,13,14,15,17,18,19,20,21,23,25,27,29,31,32, nine included surgical patients12,13,17,18,19,20,24,26,29, six included patients undergoing radiotherapy13,18,19,20,26,29, two included patients undergoing targeted therapy18,25 and in three studies, patients had immunotherapy25,27,28. One study included patients in hospice care30.
Issues faced by patients in the different treatment regimen
The included studies presented technology as a solution to different physical, mental, social, and treatment-related issues. Overall, 17 out of 23 studies covered symptom distress and side-effect management11,12,14,15,18,19,20,21,23,24,25,27,29,30,31,32,33, making it the most frequently addressed patient issue, followed by emotional distress and anxiety (n = 12)11,12,14,17,20,24,27,28,29,30,33, accurate and in-time reporting of symptoms (n = 8)18,19,21,22,25,27,30,32, communication with providers (n = 7)13,19,20,23,24,25,26,27,28,29,31,32, adherence to rehabilitation or physical activity (n = 5)20,23,24,28,29, and preparedness for treatment (n = 2)16,17,24. Intervention targets differed by treatment regimen. For instance, studies covering patients undergoing chemotherapy focused on symptom distress and side-effect management (n = 13)11,14,15,18,19,20,21,23,25,27,29,31,32, emotional distress and anxiety (n = 6)11,14,17,20,27,29, accurate and in-time reporting of symptoms (n = 6)18,19,21,25,27,32, and communication with providers (n = 6)13,19,25,27,31,32. The most common intervention focus for people undergoing surgery were symptom distress and side effect management (n = 6)12,18,19,20,24,29 and emotional distress and anxiety (n = 5)12,17,20,24,29. Studies reporting on patients who had radiotherapy reported symptom distress and side-effect management (n = 4)18,19,20,29 and communication with providers (n = 3)13,19,26 as the most common challenges addressed. Figure 4 summarizes the patients’ needs going from the most cited in the basis to the least cited in the top.
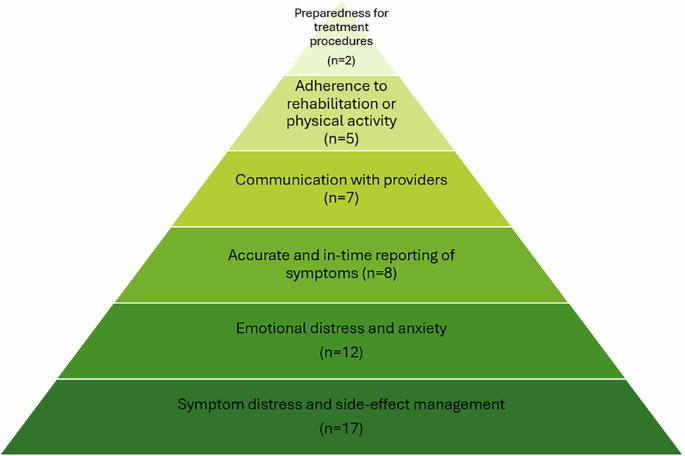
A summary of the different challenges that patients face during lung cancer treatment going from the least to the most cited challenge.
In developing study tools, the research teams either adapted commercial technologies or created specific ones tailored to their studies. Mobile applications utilized study-specific design (n = 7)18,19,21,23,30,32 and commercial tools (n = 1)31. Four of the eight telemedicine tools were designed for the study11,15,29,33, while four used commercial tools13,24,26,28. The interventions using web-based portals (n = 5) involved study-specific design (n = 4)12,16,20,27 and commercial tools (n = 1)17. Electronic questionnaires (n = 2) were designed specifically for the study22,25. One intervention used virtual reality and adopted a commercial tool14. Figure 5 illustrates how technology was utilized to meet patient needs in the pre-treatment, active, and post-treatment phases.
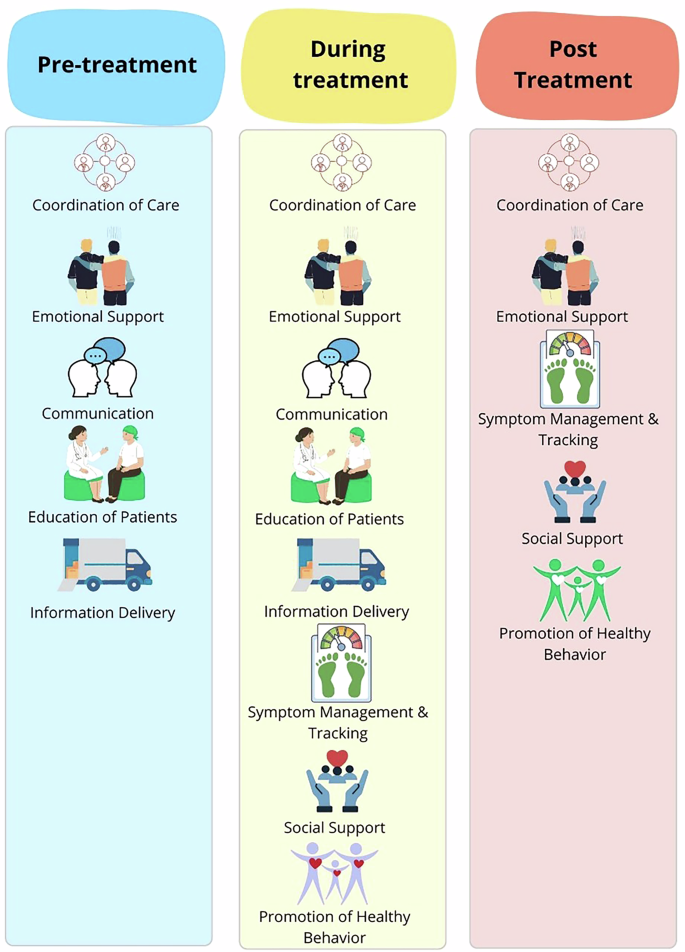
A summary of the different functions of technology in supporting lung cancer patients’ treatment in the three phases; pre, active, and post treatment.
Technology-based tools developed to support lung cancer treatment (Pre-treatment)
Technology was used to support communication and coordination, education and information exchange, and the emotional needs of lung cancer patients in the pre-treatment phase.
Telemedicine supported communication and coordination of care in the pre-treatment phase. During the pandemic, telemedicine visits for thoracic cancer patients demonstrated significant efficiency. Newly diagnosed patients seen via telemedicine reported significantly shorter median time from referral to initial visit (5·0 vs. 6·5 days, p <·001) compared to the in-person visit group, with no difference found for the time from initial visit to treatment initiation26.
Websites effectively supported education and information exchange in the pre-treatment phase. For instance, Schook et al. implemented a web-based Q&A portal called “Ask the Physician” on the Dutch Lung Cancer Information Center’s website, allowing patients and caregivers to ask lung specialists questions17. Similarly, Hopmans et al. used a patient information website for stereotactic ablative radiotherapy for early-stage lung cancer patients16. Patients reported an increased understanding of treatment and disease trajectory after using the websites16,17.
In the pre-treatment phase, websites helped reduce patients’ emotional distress. The “Ask the Physician” portal promptly responded to patients’ questions. Some patients reported reduced anxiety while awaiting their next visit in the follow-up interview. Patients also felt emotionally supported as they became more prepared for the disease trajectory and future treatment after utilizing the website17.
Technology-based tools developed to support lung cancer treatment (active treatment)
Technology supports patients in communication and care coordination during active treatment, education and information exchange, emotional and social support, monitoring and tracking, and promoting healthy behaviors.
Technologies supporting communication included electronic questionnaires, mHealth apps, telemedicine, and websites. Electronic questionnaires enhanced care coordination during patient visits. Mouillet et al. assessed the adaptation of a health-related quality of life (QoL) questionnaire with cancer patients before each visit, after which physicians prescribed supportive care (8.3%) and adapted patient management (5.2%)25. Tang et al. developed a symptom assessment tool targeting fatigue, pain, dyspnea, and anxiety, with patients reporting that the tool filled the gap in the current oncology service as symptoms were rarely discussed22. Kathi et al. conducted a randomized control trial on a mHealth application, Symptom Care at Home (SCH), that combined symptom reporting, automated self-management coaching, and follow-up calls with nurse practitioners. The SCH group showed a significantly higher reduction in severe and moderate symptoms compared to enhanced usual care. (both p < ·001)21. Two studies used telehealth in the active treatment phase to support the improvement of patients’ health-related QOL during chemotherapy15 and early palliative care11. Telehealth with a registered nurse increased health-related QOL for older adults by 8.14 points at six months (p = ·007)15. Video-based palliative care showed an equivalent effect on QoL (mean difference 2.0, 90% CI: 0·1–3·9) compared to in-person care for advanced NSCLC patients11. Several studies used web-based portals to support patients’ communication with HCPs. One study by Misplon et al. created a multidisciplinary team to support a digital portal for online follow-up and collection of patient-reported outcomes, which showed the potential to facilitate conversations between patients, caregivers, and providers27.
MHealth applications were used to educate patients in the active treatment phase. The interventions supported patients by increasing exercise capacity23, reducing symptom severity21,23, and preventing unexpected visits to emergency departments23. Park et al. provided patients with an Internet of Things (IoT) wearable device and the Smart Aftercare application, containing a comprehensive pulmonary rehabilitation program with videos for physical exercise, symptom management, and nutritional support. Patients had significant improvement on symptom scale scores for fatigue (p < ·001), anorexia (p = ·047), and diarrhea (p = ·01), but there was no significant improvement in QoL (p = 0.06) or severity of pain (p = ·24)23. The SCH app designed by Mooney et al. significantly improved patients’ outcomes since substantially less severe symptoms severity were reported for all symptoms (p < 0.001)by SCH participants compared to participants with usual care21. The MyAVL online patient portal offered personalized education materials about disease and physical activity. There was no significant improvement in patient outcome, including physical activity and quality of life20. Tang et al. provided patients with tailored symptom self-management videos. Patients reported that learning from a tablet with videos facilitated the mastery of self-management skills22.
Various technologies provided emotional support in the active treatment phase. Rose et al. used an online questionnaire, the electronic Sheffield Profile for Assessment and Referral for Care (eSPARC), with lung cancer patients to enhance follow-up care and support satisfaction. Patients reported appreciation for emotional support and reduced anxiety during the qualitative interviews13. Schneider et al. utilized virtual reality to address symptom distress during chemotherapy treatment. Patients reported an altered perception of time (p < 0.001) but no significant difference in symptom distress measured through the State Anxiety Inventory for Adults (p = ·15)14 Additionally, Misplon et al.’s digital portal increased conversations with psychologists compared to standard care. Seven out of 15 patients in the intervention arm had contact with a psychologist, while two out of 15 patients in the control arm had done so27.
Multiple studies used mobile applications to monitor patients’ symptoms in the active treatment phase. The Lalaby app by Asensio et al. collected patient symptoms through self-report and mobile sensors. They found significant correlations between app usage and emotional and symptomatic scores. For instance, the number of calls was negatively correlated with emotional scores (p = ·025) and positively correlated with the symptomatic dimension score (p = ·012)32. Patients who participated in the study on eSPARC (an electronic questionnaire combined with phone consultations) reported increased satisfaction with cancer care and QoL13. There was a 20% increase in the number of patients who reported satisfaction with the supportive care needs survey between the first and third surveys. Compared to the first and third Functional Assessment of Cancer Therapy—Lung, there was a 25% increase in patients who reported content with their quality of life13. The Kaiku Health mobile application allowed patients to report their symptoms weekly and alert HCPs about critical symptoms. Patients agreed that the use of Kaiku Health helped them to be better informed about the disease (65%), improved conversations between patients and providers (70%), and improved cancer care (51%)31. Two studies applied an integrated automated symptom reporting tool with symptom management coaching, and patients who used the mobile app showed a reduction in severe and moderate symptoms compared to the group with usual care21,30. Patients under chemotherapy who used SCH indicated significant reduction for severe (67% less) and moderate (39% less) symptoms compared to patients with usual care (both p < ·001)21. For patients in hospice care and caregivers supported by the same tool, SCH produced a symptom reduction of 4·89 severity points (95% CI 2·86–6.92, p < ·001)30.
Park et al.‘s mobile application has a pulmonary rehabilitation program and access to symptom management resources, and it is linked to an Internet of Things wearable device23. It improved the exercise capacity of the patients, as patients had a significant increase in score for the 6-minute walk test (6MWT) at 6 and 12 weeks (both p < ·001)23. Telemedicine was applied in multiple studies to promote rehabilitation for patients in active treatment. Loy et al. created a Virtual Integrative Oncology Shared Medical Appointment Series (VIOSMAS) that covered various topics, including nutrition, culinary arts, herbs/botanicals, exercise, narrative medicine, etc. Patients could incorporate recommended lifestyle changes, and they reported that the tool addressed and improved symptom distress, including sleep, fatigue, anxiety/fear, gastrointestinal symptoms, and pain/weakness in the post-session assessment, while no direct measure on patient outcome was reported33. The PACTIMe-FEAS study by Charlet et al. applied telehealth sessions on physical activity, finding a significant 2.1-point mean decrease in fatigue (p = ·0161)28. Lastly, MyAVL, an online patient portal, provided tailored physical activity support to patients, but we did not find any significant improvement in patient outcomes20.
Technology-based tools developed to support lung cancer treatment (Post-treatment)
In the post-treatment phase, patients’ support consisted of monitoring and coordination of care, emotional and social support, and promotion of healthy behavior.
Mobile applications play a crucial role in post-treatment care and early relapse detection. Denis et al. randomized patients to use a mobile application, “sentinel,” or regular follow-up post-treatment18. Similarly, another team of researchers in France performed a randomized trial to compare patient outcomes using a web-mediated follow-up algorithm with regular surveillance19. The two applications required the patients to complete a weekly symptom self-assessment form between follow-up visits. The app sends real-time data and alerts oncologists of alarming symptoms of relapse. Subsequently, the medical team adjusted the current supportive care and organized imaging and follow-up visits18,19. Denis et al. found that the median survival time was significantly longer for patients using the sentinel app (22·4 months) compared to patients who received regular follow-up (16 months, p = ·0014)19. The algorithm study found that the median overall survival was 19·0 months for the experimental group compared to 12·0 months for the control group (p = ·001). There is a significant difference in the number of patients who initiated optimal treatment in the experimental arm compared to the control arm (p < ·001)18.
Li et al. explored a telemedicine program’s efficacy for lung cancer patients with chronic post-surgical pain. Patients were randomized to receive treatment and psychological support in person or via the Internet. There were no significant differences in the QoL or the satisfaction rate in the group with in-person care versus the group with telemedicine (p > ·05)12.
Several studies have used telemedicine to support patients in post-treatment rehabilitation. Li et al.’s program educated patients on lifestyle adjustment and pain management12. Ha et al. delivered a 12-week intervention on exercise training, education, and behavior change to lung cancer survivors29. The research team found significant improvement in the health-related QoL measured by the St. George’s Respiratory Questionnaire of patients who participated in telemedicine intervention compared to the control group at baseline (standardized effect size: −1·03 to −1·30)29. In contrast, Li et al. found no difference in QoL for patients in the telemedicine group compared to patients who received in-person care assessed by the 36-Item Short Form Health Survey(SF-36) (p > 0.05)12. Lafaro et al. discovered that telehealth sessions on occupation and physical therapy improved the functional capacity measured by 6MWT by 6 points, while the difference was not significant compared to baseline (p = ·70). However, patients showed significant improvement in short physical performance battery score compared to baseline (p = ·01)24.
Barriers to technology use for treatment support
The studies also reported various technological barriers, including low digital skills, confusion and information overload, cost, access to technology, preference for in-person care, and reliability regarding electronic reporting. Access to technology was one of the most prevalent challenges highlighted by the studies18,21,26,28,29. This included barriers such as unreliable phone signals29, difficulty accessing and affording the Internet, and access to digital devices like smartphones21. Low digital literacy was a significant concern, as some patients struggled with navigating tools and understanding content and required setup assistance due to limited experience or competence with technology18,19,20,22,25,27,31,33. Complex visual representations, complicated login processes, and limited compatibility with specific operating systems exacerbated these challenges20. Confusion and information overload emerged as another challenge, with participants feeling overwhelmed by excessive information, leading to reduced technology use17,24. In a few studies, patients preferred in-person care, citing challenges with remote instructions and greater comfort with in-person interactions compared to internet-based alternatives12,17. Finally, reliability regarding reporting was an issue, as some patients found it difficult to accurately report their symptoms or align their perceived quality of life with structured questionnaires22,32. These themes highlight the multifaceted barriers to effective technology use in healthcare, emphasizing the need for improved accessibility, support, and user-centered design.
link







